Unlock more profits with DoorDash
Delivering more
When you think of DoorDash, you think of delivery — but the DoorDash Merchant Suite delivers many ways to help you grow.
Grow with DoorDash
Expand your reach by listing your business on the DoorDash app, also known as Marketplace. Plus, increase sales by tapping into DashPass subscribers, who spend and order more on average. Included in every partnership is Storefront — customizable and commission-free online ordering that lives on your website. Or use Drive to offer delivery from your own app or site by tapping into DoorDash’s network of Dashers. Finally, streamline operations with Bbot, our in-store digital ordering and payment solution.
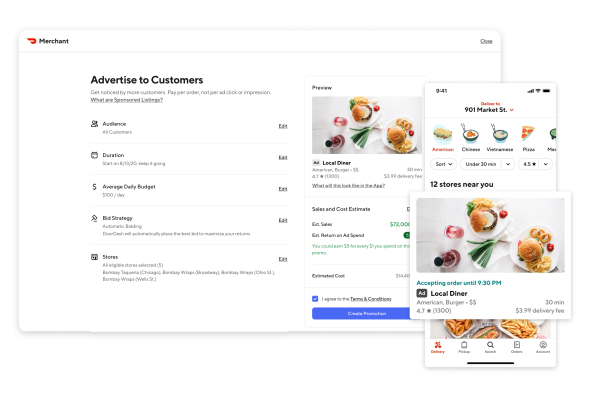
Attract new customers
Sponsored Listings give you prime real estate in the DoorDash app so you get noticed by new customers. Promotions let you offer discounts or free items to encourage customers to place orders, and Storefront promotions use similar incentives to get customers to place commission-free orders directly on your website. Brand Licensing lets you add a revenue stream by selling an established, well-known brand out of your restaurant’s kitchen.
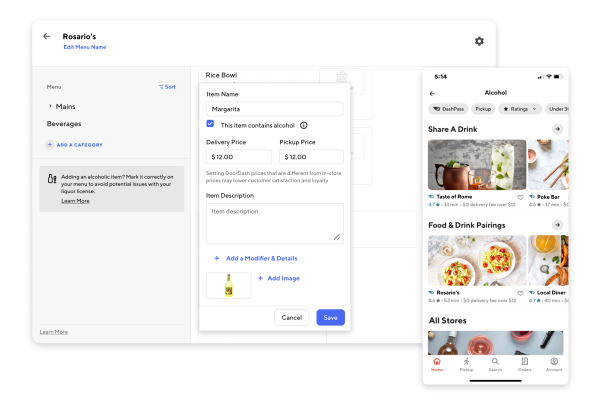
Increase order volume & size
Increase order volume and size (and, as a result, profits) with Promotions that provide customers with discounts or free items only when they reach a specific minimum order size. If you already offer beer, wine, liquor, or cocktails in-store, add alcohol to your DoorDash menu to help increase ticket sizes and reach customers looking to order both food and alcohol.
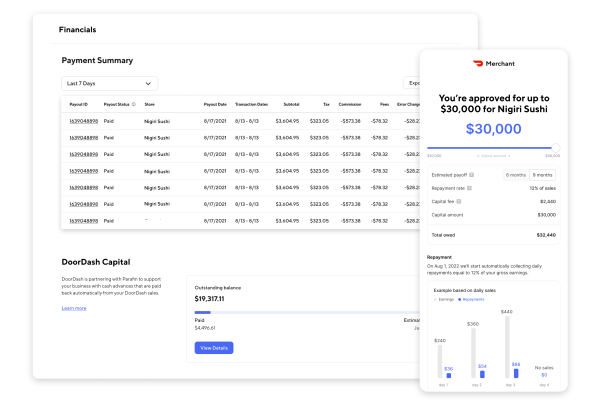
Access financing
Take your business to the next level by expanding with DoorDash Capital. Easy, accessible financing can help eligible merchants invest in new equipment, open a new location, hire more employees, and much more.
"The additional revenue that we receive from DoorDash is very helpful. Not only does it provide more sales, but the incremental margins on those sales are a lot higher because we've already covered our fixed costs with our regular business."
Jamie Schrotberger, CEO, Spread Bagelry
Take our short quiz to identify the right solution for you
Which of these is more important to you?
"[DoorDash has] definitely gone above and beyond in terms of helping us whenever there's any issues — and more so than that, they've helped us a lot in terms of marketing, branding, and getting the word out about Favorites."
Jonathan Poon
Owner, Favorites Thai BBQ

We’re committed to strengthening neighborhoods
Since our founding in 2013, DoorDash Marketplace has generated over $100 billion in sales for merchants.

Get the most out of DoorDash
We provide customized, accessible support whenever you need it, including 24/7 phone and chat support, account help, and direct communication with assigned drivers.
Plus, visit the Learning Center to view step-by-step tutorials and training videos on setting up, running, and growing your store on DoorDash, so you can grow profits and reach more new customers.
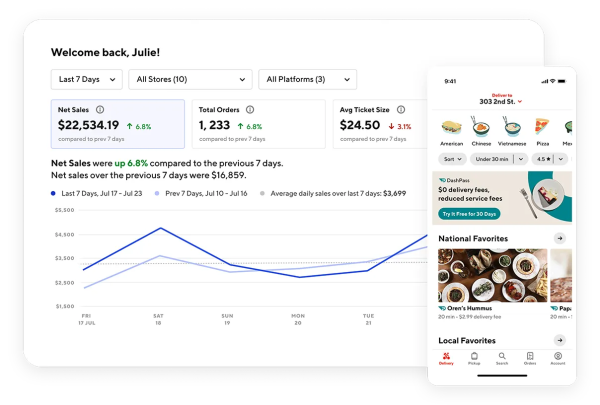
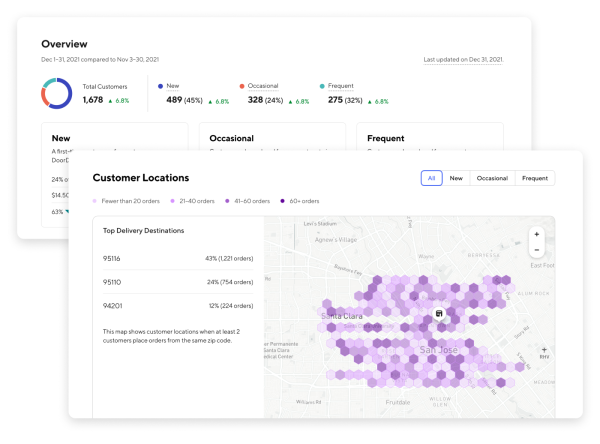
Explore insights you can use
Analyze sales, access financials, respond to reviews, and check out customer insights including zip codes for delivery. Log on to the Merchant Portal or use the Business Manager App on your phone.
Access opportunity, capital, and community
We’ve developed a number of initiatives to support you, your business, and the causes you care about.
Frequently Asked Questions
Pricing plans differ based on the level of built-in marketing plans included.
The "Basic" including our core marketing tools (listing your business on the DoorDash app, discoverable in search, and featured in our algorithmic collections like "Fastest Near You" or "Local Favorites") at 15% delivery commission and 6% pickup commission with a 7-day free trial.
The "Plus" plan adds an expanded delivery area and DashPass, at 25% delivery commission and 6% pickup commission, with a 30-day free trial.
The "Premier" plan includes all of the benefits of "Plus" and a Growth Guarantee* at 30% delivery commission and 6% pickup commission, with a 30-day free trial.
All plans include Storefront, commission-free online ordering for your website.
Partnership Plans are available for restaurants with 75 or fewer locations in the US. 6% Pickup is available to all partners in the US who comply with the DoorDash Merchant Terms of Service, including having DoorDash Pickup menu prices match in-store prices.
Commission is a percentage of the order subtotal for each order processed through the DoorDash platform. DoorDash charges commission rates to bring value to your business and community; commissions cover advertising and marketing, delivery driver costs, customer service for consumers, merchants, and Dashers, technology platform costs, and more. Learn more about pricing.
*DoorDash "Premier" Growth Guarantee: Accept at least 20 orders per month or DoorDash will refund your commission costs for that month. Partners are eligible for this rebate only if (1) they cancel fewer than 5 orders that month and (2) maintain "open hours" on DoorDash for 90% of the Store Hours that they have set in the Merchant Portal.
DoorDash does not charge an activation fee, subscription fee, software fee, cancelation fee, contract fee, or any hidden fees. However, certain fees may be applicable for additional products or services as you opt in, such as:
If you choose to use the DoorDash Tablet to accept orders, you can use it for free for the length of your trial, then $6 per week in the US, $3 per week in Canada, and $0 per week in Australia and New Zealand. You can also accept orders via point of sale integrations, email, or fax at no cost to you.
Marketing fees if you choose to use Promotions or Sponsored Listings to grow your sales.
Payment processing fees only for Storefront orders, which are commission-free.
DoorDash charges fees and commission rates to bring value to your business and community. Here are some of the items they cover:
Advertising and marketing: Being on the DoorDash app puts your business in front of new customers every day.
Delivery driver costs: We empower our community of Dashers, who make every delivery possible, by providing them flexible earning opportunities with competitive local pay, promotional pay, 24/7 support, third party insurance, and exclusive discounts. Learn more about the Dasher Community at Dasher Central.
Customer service and support for consumers, merchants, and Dashers: Customers, business owners, and Dashers all have unique needs that often need addressing immediately. When something goes wrong with an order, we have a 24/7/365 team of people ready to help solve customer issues, so they’ll continue to order from your business.
Technology platform costs: It takes a world-wide, world-class logistics, engineering, coding, marketing, and operations team to keep the DoorDash app and website, our Merchant Portal and tablet, and our Dasher app running. We hire the best and expect the best from our team.
Credit card processing: With the exception of Storefront (where you only pay a credit card processing fee* with no additional commissions, monthly fees or per-order fees), all DoorDash offerings include credit card processing, so you have less to worry about when it comes to overhead expenses.
*2.9% of the total transaction amount + $0.30 per order
You can change your plan any time in the Merchant Portal. Plans may take 5 business days to process changes, so it is not feasible to change your plan more often than about one time per week.
We encourage merchants to try a plan for a minimum of 2-3 weeks before switching in order to get the most representative picture of how well each plan works for your business.
Merchant partners can either choose to receive a weekly direct deposit from DoorDash or opt in to daily payouts at no charge.
In the US and Canada, DoorDash Basic partners start with a 7-day free trial, and DoorDash Plus and Premier partners start with a 30-day free trial. This means delivery and pickup commissions are 0%, so you can try the partnership plan* that works best for you. Tablet fees are also $0 for the duration of the trial. After the trial, there is a weekly tablet fee of $6 in the US, $3 in Canada, and $0 in Australia. Point of sale integrations are free.
After your free trial, you’ll be enrolled at the commission and tablet fees indicated in your "Merchant Signup Sheet."
You can change your plan at any point in your trial (and after your trial) within the Settings in the Merchant Portal.
*Partnership plans (Basic, Plus, Premier) are available for restaurants with 75 or fewer locations in Canada or the US.
If you switch plans in the middle of your trial, your free trial ends, and you will be enrolled in your new plan, paying that plan’s commission rate, within the next 5 business days. If you do not want to end your free trial early, we suggest setting a calendar reminder and logging in to update your plan 5 or fewer days before your trial ends.
Yes, you can opt out of your free trial at any time. Please reference this resource to learn more.
If you'd like to speak to a merchant sales representative, you can contact us online or call us Monday-Friday:
United States and Canada: 855-554-5779
Australia: 1800-717-576
Already a DoorDash merchant? Browse help.doordash.com for answers to your questions, explore the Learning Center, or call merchant support:
United States (English and Español): +1-855-222-8111
Canada (English): 647-957-7219
Canada (Français): 855-643-8439
Australia: 1800-958-316
New Zealand: +64-800-001-188









